Dying or Lying? For-Profit Hospices and End of Life Care
AHEC, April 28, 2023
Background
What is hospice?
National Cancer Institute Definition
“A program that gives special care to people who are near the end of life and have stopped treatment to cure or control their disease…The main goal of hospice care is to control pain and other symptoms of illness so patients can be as comfortable and alert as possible. It is usually given at home, but may also be given in a hospice center, hospital, or nursing home.” emphasis added
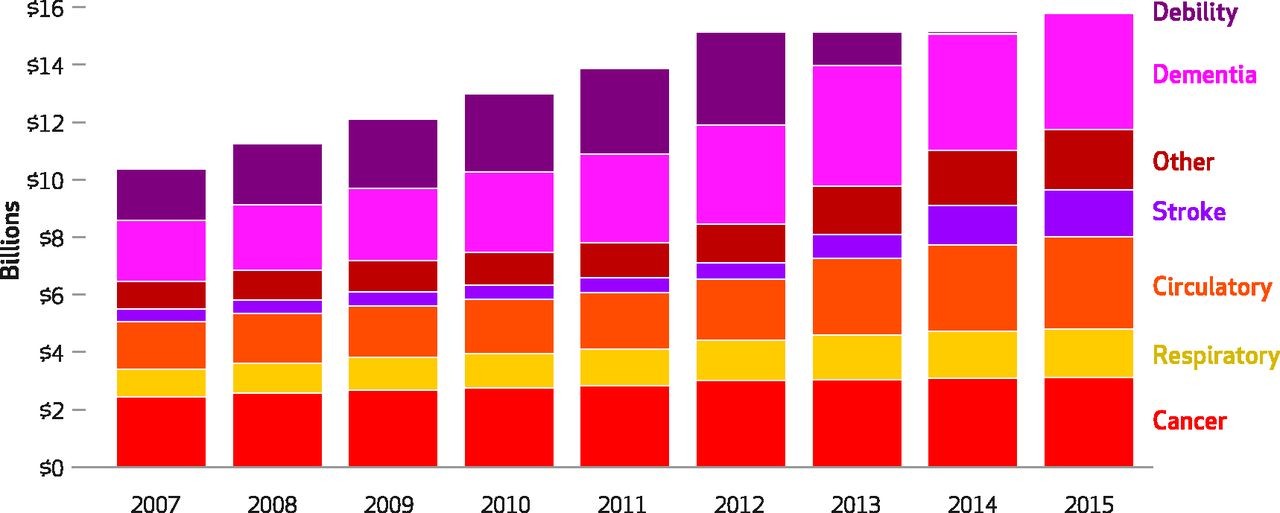
Hospice spending
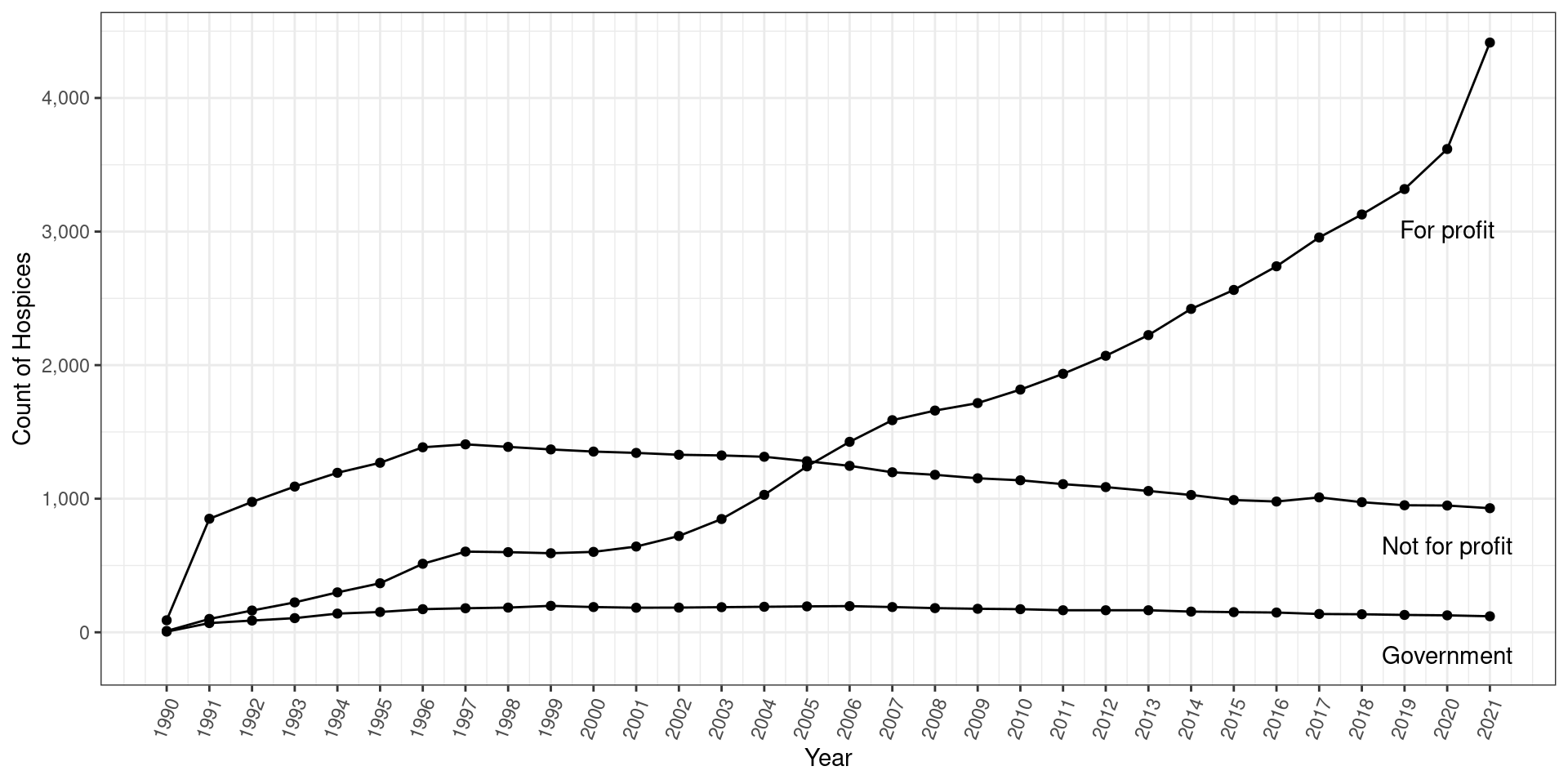
Growth of for-profit hospices
Malleable admission criteria
- Eligibility: Life expectancy < 6 months
- Over 20% live beyond 6 months
- Nearly 30% among FP hospice
- Half of ADRD hospice patients live beyond 6 months
Summary
- Big increase in hospice spending
- Substantial growth of for-profit hospices
- Potential exploitation of imprecise admission criteria
Research Question
What does growth of FP hospices mean for total health care spending and health outcomes? Do policies intended to curb improper admissions actually work?
What does this paper do?
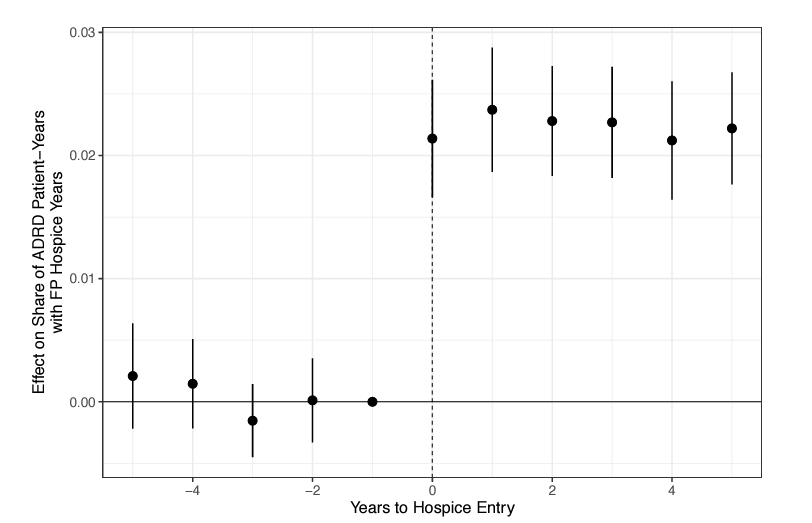
Empirical strategy
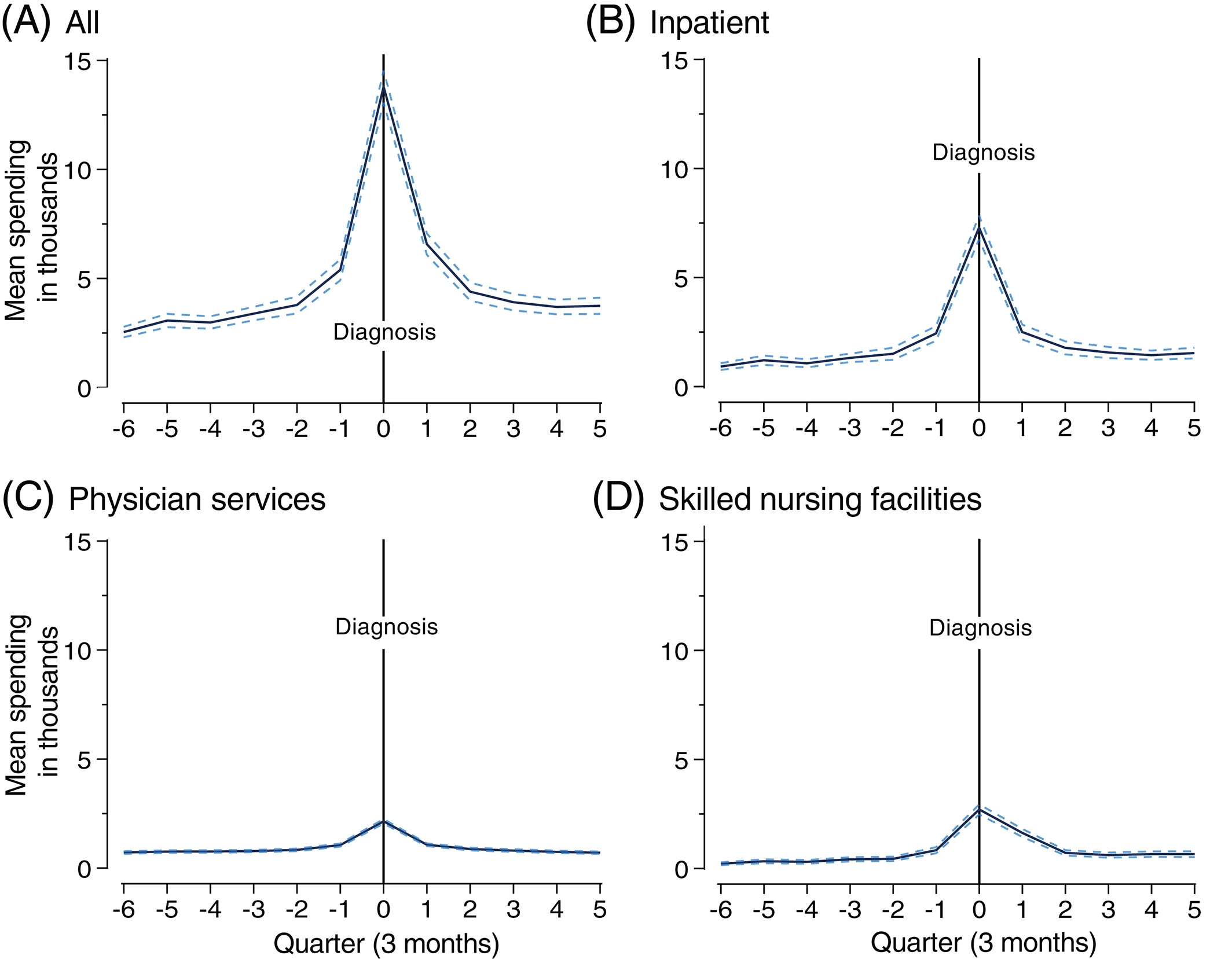
- Focus on ADRD diagnosis without restriction to people that die within certain time period
- Examine spending and mortality over 5-year period
- 2SLS using FP distance as instrument
\[ \begin{align*} FP_{icz} &= \alpha + \beta \mathbf{D_{FP,cz}} + \delta X_{icz} + \gamma D_{NP,cz} + \lambda_{z} + \lambda_{c} + \epsilon_{icz} \\ Y_{icz} &= \tilde{\alpha} + \tilde{\beta} \widehat{FP}_{icz} + \tilde{\delta} X_{icz} + \tilde{\gamma} D_{NP,cz} + \tilde{\lambda}_{z} + \tilde{\lambda}_{c} + \varepsilon_{icz} \end{align*} \]
Empirical strategy
- Identification from variation in spending for different patients within same zip code
- “Pre-period” patients were in the same zip code but FP hospice was further away
- Decomposition of MFX between “otherwise NFP” and “new” hospice patients
Findings
- Large spending reduction:
- $44,000 relative to no hospice, small and insignificant relative to NFP
- Increased mortality:
- 30% (4 percentage points) 90 days from diagnosis
- 25% (6.8 percentage points) 1 year from diagnosis
- 13% (8.6 percentage points) 5 years from diagnosis
- Larger effects relative to no hospice, null effects relative to NFP
Some conceptual questions
“Traditional” spending on ADRD patients
Direction of effects guaranteed?
- By definition, hospice patients forego curative care
- Sending all elderly ADRD patients into hospice would seem to save money and increase mortality
- Critical question is where new patients are coming from and how
New FP patients come from:
- Patients otherwise going to NFP hospice
- Unmet need due to capacity constraints
- Unmet need due to information problems
- Patients not otherwise seeking hospice (induced to hospice)
Diagnosis for hospice
Not only admission that is potentially influenced by presence of FP hospice
Diagnosis for hospice
Not only admission that is potentially influenced by presence of FP hospice
Hospice organizations can assist in determining eligibility for patients suffering from terminal illnesses.
Some empirical questions
Does change of ownership matter?

Distance as an instrument
- Firms locating somewhat strategically
- Presumably partly due to proximity to patients and competitors
- Are FP hospices just locating in under-served areas, where the only other care option is inpatient care?
- Concern made worse when conditioning on NFP distance
Balance on observables
- Some differences in diagnoses
- kidney disease
- diabetes
- hyperlipidemia
- hypertension
- Large racial differences (90.3% white versus 83.6%)
- Urban vs rural?
Final thoughts
In consideration of “new” hospice patients:
- Effects among baseline capacity constrained and unconstrained markets
- Lower spending almost guaranteed (?), but mortality effects seem potentially large
- Measure ex post change in spending and mortality if everyone of a certain age/diagnosis stopped receiving curative treatment
- Are FP hospices identifying patients on the “better” end of this distribution?
Distance as IV:
- Preliminary matched/weighted DD estimates using FP entry as treatment
- Sensitivity to NFP distance in 2SLS estimates
- Consider “plausibly exogenous” bounds
Takeaways
- Great question with important policy implications
- Interesting welfare question regarding mortality effects
- To policy makers…
- If you want to encourage or discourage something specific, tie incentives directly to that specific thing
Thank You!
Ian McCarthy, Emory University & NBER
ianmcccarthyecon.com
ian.mccarthy@emory.edu